The birth of this initiative dates back to the last years of the past century and Tampere, where Drs. Pekka Kannus and Harri Sievänen took on the challenge of addressing the “growing epidemic” (surge in the number) of osteoporotic fractures. Contrary to then-persisting – and sadly, still persisting – view that fractures of older adults were due to bone fragility (osteoporosis), Drs. Kannus and Sievänen published a series of studies that convincingly showed that these fractures are primarily due to falling – not osteoporosis.
Following on this rationale that fractures are primarily due to falling, a research team led by Pekka Kannus first developed a scientifically sound hip protector:
Then showed that people were ready to wear it (the developed device had acceptable compliance): And then, finally went on to establish that this device could effectively prevent hip fractures:
And then, finally went on to establish that this device could effectively prevent hip fractures:
At this highly productive period, Dr. Järvinen was working as a PhD student in this research group led by Drs. Kannus and Sievänen. Inspired by these groundbreaking studies, he decided to follow on this somewhat unconventional path in the field of osteoporosis.
This long and winding road led to the following discoveries – or intellectual paradoxies – as they have been coined by the researchers who have been involved in these studies:
Paradox 1: DXA is an uncontested diagnostic tool for assessing “bone mineral density”, but when placed under proper scientific scrutiny, fails horrendously.
In this extensive series of dual-energy X-ray absorptiometry (DXA) scans and dual polyenergetic X-ray simulation studies of 150 different phantom arrays carried out to evaluate quantitatively the extent of systematic inaccuracies inherent in DXA in vivo bone mineral density (BMD), we found that BMD inaccuracies as high as 20% or more can be readily anticipated clinically, particularly in cases of osteopenic, osteoporotic, and elderly patients. Of note, we tested all available DXA scanners (i.e., Hologic, Lunar, and Norland densitometers) and the inaccuracies were found to be virtually the same irrespective of the scanner used.
The clinical relevance of this uncertainty can be explained as follow: The magnitude of the effect of this error is analogous to getting a standard arm cuff blood pressure recording of 160/100 mmHg and realizing that with similar uncertainty, the true value could lie between 140/88 and 180/112 mmHg.
How comfortable would you be making treatment decisions on a patient with elevated blood pressure if your measurement was this shaky?
Paradox 2: Bone quality
Bone quality was a widely embraced concept in 2005, as it was said to offer a solution to the classic paradox of osteoporosis: while low BMD values are associated with increased relative risk of fracture at the population level, the predictive value of BMD in an individual patient remains quite marginal. The National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS) and the American Society for Bone and Mineral Research (ASBMR) even hosted a special conference on this topic, entitled “Bone Quality: What Is It and Can We Measure It?” at the NIH (Bethesda, MD, USA) on May 2-3, 2005.
The new concept made absolutely no sense to us.
To succinctly explain our concern: As the whole bone strength provides the ultimate measure of true bone quality, the paradox of osteoporosis appears to simply stem from our inherent inability to determine directly the actual bone strength of an individual in vivo. However, this inability cannot be taken as a justification to introduce an obscure and ill-defined concept such as bone quality.
We wrote two papers, one published in the flagship open access journal PLoS Medicine, arguing that the entire concept “bone quality” is an “empty term” – similar to Emperor’s new clothes in the famous fairy tale.

After a surge in popularity in the early years of the 21st century, the term “bone quality” has fallen into disuse.
Paradox 3: Fractures are due to falling, not osteoporosis
As noted, Dr. Kannus’ seminal work had already established that fractures in the older adults are primarily attributable to falling, not osteoporosis. This being the case, a paper had to be written about how to prevent falls. Typical of Pekka Kannus’ work, he went on to publish a number of articles in some of the most prestigious general medical journals:
Despite this evidence (N.B., that has never been refuted!), the majority of healthcare professionals opted to stick to the “old truth” of preferring to tackle the impeding fracture epidemic through efforts aimed at boosting bone mass or preventing bone loss (osteoporosis).
What now?
There seemed to be no other option, but to write more papers calling out the above noted issues. The first in a series of current three BMJ Analyses was a comprehensive review that highlighted that we should be putting our efforts into stopping falls – not treating low bone mineral density (osteoporosis).

The paper proved to be a major (intellectual) paradigm shift that led to attention from most international news media (e.g., the BBC, BBC radio, CNN, as well as majority of Finnish news media). In certain parts of North America, the osteoporosis guidelines began to include fall prevention as a critical element (e.g., British Columbia Bone Health Guidelines 2011, Canada).
We were thrilled to note that the prestigious BMJ also valued our contribution, posting falls prevention as their cover story:
Together with a paper by Pablo Alonso-Coello, Ray Moynihan and Gordon Guyatt (https://www.bmj.com/content/336/7636/126), our Analysis piece have become an influential pair in resisting disease mongering in osteoporosis. Alonso-Coello and colleagues called attention to the widening of disease definitions in osteoporosis by the introduction of the concept “pre-osteoporosis”. Another new concept that made absolutely no sense to them or us (but apparently made to a lot of people working in the field). Another concept that has fallen into disuse.
Paradox 4: Preventive pharmacotherapy is not feasible
Another three years and it was time to rock the osteoporosis cradle again with our second BMJ Analysis. This article built on the above noted 2008 paper, but now extended from the prevention and treatment of fractures to challenge the feasibility of preventive pharmacotherapy in general. In fact, the paper challenged the prevailing claims on the “cost-effectiveness” of preventive pharmacotherapy trumpeted by expert panels in many medical disciplines (e.g., statins and anti-hypertensives in the prevention of cardiovascular disease and bisphosphonates in the prevention of fractures).
We articulated the fundamental problem with the current cost-effectiveness models that the data underpinning the efficacy of the drug do not reflect clinical practice. In essence, the models extend the highly specialized evidence on drug efficacy as if it were widely applicable in community practice. In economic jargon, the prevailing data that are proposed are merely one element of a sensitivity analysis – and the very favourable elements at that.
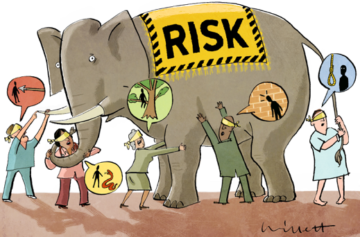
This was also the first time that we teamed up with the legendary BMJ artist Malcolm Willett. We asked Malcolm if he could consider thinking of producing artwork for our paper. After reading our manuscript, Malcolm emailed us this fantastic art that truly captures the essence of our paper!
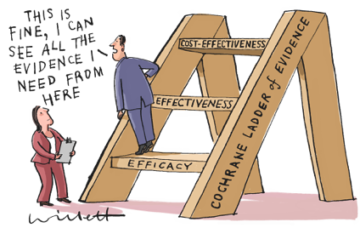
We are not the only ones who thought highly of the image, as it was later published in the cover of the British Journal of Sports Medicine, the highest ranked journal in Sports Medicine!
Paradox 5: FRAX – A fragile fracture risk prediction tool that was fraught with errors and malicious scientific practice
But the advocates of the prevailing “osteoporosis-focused” prevention strategy weren’t ready to abandon their “low BMD / osteoporosis” darling. As the foundations of their story were about to crumble into dust – one keystone after another – the field made a major shift in focus: From a surrogate (low BMD) to “high risk of fractures”.
Along came the fracture prediction tools. To those who have followed the evolution of other “major non-communicable disease”, this re-make of treatment target did not come as a big surprise – exactly the same “shift” had taken place in the fields of hypertension, hypercholesterolemia, and type II diabetes!
Sadly, the osteoporosis community adopted this change with no need for solid evidence. While building evidence to challenge the strategy, professors Karl Michaelsson (Uppsala University) and Gary Collins (Oxford University) published a critical piece that dissected the FRAX tool, highlighting/showcasing all the flaws related to the performance of the tool: FISCAL teamed up with these world-leaders on osteoporosis/fracture prediction, to scrutinize other concerning issues related to the FRAX tool. This collaboration resulted in a Commentary published in the CMAJ with a title that capture the essence of our disturbing findings:
FISCAL teamed up with these world-leaders on osteoporosis/fracture prediction, to scrutinize other concerning issues related to the FRAX tool. This collaboration resulted in a Commentary published in the CMAJ with a title that capture the essence of our disturbing findings:

In brief, we expressed concerns about the development and promotion of FRAX, including lack of transparency about the underlying equation, use of one codeveloper’s “own journal” to promote and defend it against critique, and apparent violations of guidelines for handling conflicts of interest.
Two years later (December 2017), the WHO published an editorial in the Bulletin of the World Health Organization titled “Clarifying WHO’s position on the FRAX tool for fracture prediction”, with a following notion:
By this statement, the World Health Organization wishes to make clear that the FRAX® tool to evaluate fracture risks of patients is not a “WHO tool” and has not been developed, endorsed, evaluated or validated by WHO, notwithstanding any public statements and claims to that effect…Furthermore, according to our records, WHO has not authorized the use of the WHO name, acronym or emblem in connection with the FRAX® tool, including for the tool’s branding, promotion or sale.
http://www.who.int/bulletin/volumes/94/12/16-188532/en/
Although it took the WHO more than two years to act, I guess we were right after all. Funnily, this statement has completely escaped the attention of the bone journals although even such journals as the New England Journal of Medicine posted this statement on their pages:
https://www.nejm.org/doi/full/10.1056/NEJMc1715766
Paradox 6: Overdiagnosis of bone fragility…
With all the new evidence, but little change in contemporary clinical practices, the FISCAL team decided to write yet another paper to gather all the information together related to the screening and treatment of individuals at risk of fractures. Coincidentally, the BMJ had just launched a new campaigned coined “Too Much Medicine”. Immediately, it seemed like a perfect fit for our paper.
With the help of our old collaborators and a few new ones (from Therapeutics Initiative, at University of British Columbia, Canada, and from Spain), we took on the task. If possible, this 3rd BMJ Analysis turned out to be the most difficult of the three Analyses on osteoporosis: numerous reviewers, numerous rounds of revisions, editing to address the reviewers’ criticism … all of a sudden, we realized that so much great material had to be left out from the concise BMJ Analysis. We actually had material for another paper…
While working on the BMJ revisions, Dr. Järvinen received an invitation from the Roayl Swedish Academy of Sciences and the Journal of Internal Medicine (JIM) to give a talk at the 11th Key Symposium on “Molecular and clinical prediction of the risk for osteoporotic fractures”. Dr. Järvinen’s talk was entitled “Dismantling the Osteoporosis Bomb”
As a part of the invitation, all keynote speakers were offered a chance to publish a commissioned Review article in the Journal of Internal Medicine. We now had a venue for our other paper, too. Or at least we thought so.
Not surprisingly, the publication of these two papers turned out to be laborious crusade. But persistence paid off, again, as our Too Much Medicine BMJ Analysis was published in 2015:

BMJ treated us very kindly: Our piece made their cover again.

The other paper was also finally published in the same year, but not before quite a bit of “persuasion” (for example, we needed to remind the JIM what it means to have “commissioned” a paper and what it means to have a “balanced and evidence-based review of a manuscript”):
The JIM paper proved very fruitful, as it not only allowed us to air out our concerns more comprehensively than in the BMJ, but it also enabled an opportunity to publish another set of Malcolm Willett’s images:
 and
and 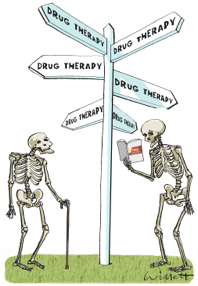
It came as no surprise to us that our peers were not thrilled by these two publications. In fact, the major osteoporosis advocacy groups/bone organizations sent their responses to the BMJ and encouraged their supporters to do the same. The BMJ “mailbox” was filled with rapid responses criticizing our paper (https://www.bmj.com/content/350/bmj.h2088/rapid-responses).
The advocacy organization even saw the trouble of publishing their counterarguments in their own websites and in their journals:
- ASBMR statement in response to British Medical Journal paper published on May 6, 2015 and Jounal of Internal Medicine paper published online May 25, 2015
-
IOF response to recent articleon overdiagnosis of bonefragility
- ISCD Response to Controversial Editorial in the British Medical Journal
The following statements were made about our paper:
- “inflammatory”
- “The article distorts and grossly misrepresents the osteoporosis burden”
- “confuse and mislead the public and the medical community with inaccurate and harmful conclusions”
- “deem[ed] inaccurate and misleading on a number of levels”…
What came – and still comes – as a great surprise to us: Despite apparently having such influential papers that they required an abundance of comments to be submitted, critique to be expressed and “bold” statements to be made, none of us authors of these two publications have ever been invited to a bone meeting to discuss our facts! In fact, Dr. Järvinen once agreed on a scientific debate to be held in Jordan and an opponent was already named, only to have the debate cancelled later on the grounds of “…failing to find somebody interested to share in this debate”.
Paradox 7: Understanding risk: Are blind leading the blind?
Nowadays, being at ‘high risk’ of having a disease has become a disease in and of itself. Sweeping educational programmes at all levels of healthcare now turn an otherwise healthy person’s ‘high’ blood pressure, elevated serum lipids or low bone density into chronic conditions having increased risk of a potentially bad event.
But what represents ‘high risk’?
This question lies at the heart of modern medicine, particularly with respect to pharmacological primary prevention. And this is what the next FISCAL publication addressed:
The main message of the paper? Both doctors and patients are equally risk illiterate – neither has a glue what represents “high risk”.
Malcolm was again kind enough to come up with an image that captured the essence of the story:
Where are we now?
15 years of hard work, a good number of publications, a huge number of different collaborators around the world with one common feature: an aspiration or even an obsession for truth.
But has anything changed?
No. And yes.
We take pride in being among the growing number of people who have realized that the prevailing prevention and treatment strategy for elderly fractures of relying on boosting bone mass through osteoporosis drugs does not stand scientific scrutiny.
We have also witnessed a roughly 50% decline in the number of people taking osteoporosis medications. Obviously, we can’t take credit for this change, but feel that we have been among the few research groups trying to air out the above noted concerns regarding the prevailing treatment strategy for osteoporosis and fractures in the older adults.
This story continues. Stay tuned, interesting projects in the pipeline with old collaborators and some new ones!